Antidepressants have long been prescribed globally to people grappling with depression and anxiety.
Yet, recent studies and critiques are casting shadows on their purported benefits and uncovering possible risks associated with their long-term use.
A paper published in Epidemiology and Psychiatric Sciences discussed the overarching assumption that depression stems from specific brain chemical imbalances, which antidepressants can allegedly correct.
However, evidence suggests that these medications might not normalize brain function but rather disrupt biological processes, sometimes leading to grave consequences.
Scientists are still unraveling the immediate neurochemical changes induced by antidepressants and how the body’s long-term adaptation to these drugs manifests.
Historically, it has taken the medical community considerable time to acknowledge drug-induced side effects, such as tardive dyskinesia from antipsychotics or the alarming withdrawal symptoms from antidepressants.
Withdrawal reactions signify that the body undergoes significant alterations due to drug ingestion.
These effects can occur even after a single dose, with many facing prolonged withdrawal symptoms that may last for months or even years.
This parallels the well-documented benzodiazepine withdrawal symptoms and the persistent withdrawal syndromes sometimes experienced after stopping antidepressants.
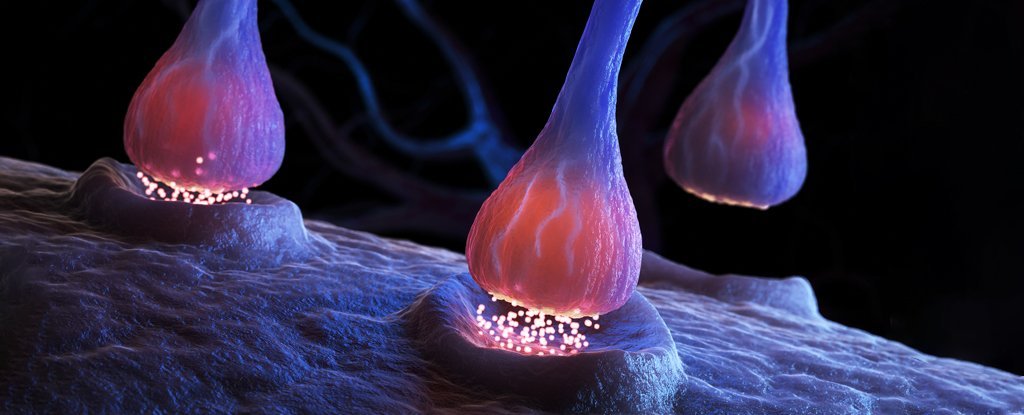
Another rapidly growing concern is post-selective serotonin reuptake inhibitor (SSRI) sexual dysfunction.
SSRI drugs, often prescribed for their mood-enhancing properties, have been linked with persistent sexual dysfunction even after patients stop taking them.
Studies, including those conducted on animal models, suggest a lasting impact, emphasizing the need for rigorous and well-funded research to understand these effects fully.
A recent study led by Copenhagen University psychologist Vibeke Dam and colleagues further complicates the picture.
The study involved 90 patients with moderate to severe depression, who underwent brain scans and cognitive and mood assessments before and after taking the SSRI escitalopram.
Results showcased almost a 10% reduction in the cell receptors targeted by the SSRI and improvement in memory cognitive tests, specifically in verbal recall.
However, intriguing findings revealed that those with minimal changes in a specific serotonin receptor (5HT4) showed the most improvement in verbal memory, yet these receptor changes did not correlate with mood improvements.
These results led researchers to speculate that SSRIs may increase efficiency in remaining serotonin receptors, which could boost cognitive function.
Despite these findings, the absence of mood improvements linked to receptor changes raises questions about SSRIs’ role in addressing depression.
Additionally, ethical restrictions have limited the use of placebos in such studies, casting further uncertainty on the outcomes observed.
Given the high dependence on antidepressant medications, it remains essential to recognize the benefits and potential risks these drugs entail.
For instance, antidepressants’ effects might not always align with their intended purpose, and conflicting studies continue to debate their efficacy over placebos.
Important future directions for research should aim to uncover the precise mechanisms through which these drugs operate and how they might be optimized or replaced in treating mood disorders.
While these insights cast doubt on the efficacy and safety of long-term antidepressant use, it’s crucial for patients currently on these medications to consult their doctors before making any changes.
As researchers suggest, a deeper understanding of antidepressant mechanisms and alternative treatments could significantly improve precision psychiatry for those suffering from major depressive disorder.
As we move forward, continued research and better-funded studies will be vital in advancing our understanding of these widely used medications and ensuring safer, more effective treatment strategies for mental health.
